Coronavirus update: Change in testing strategy
As the virus is now more widespread in the Danish population, the health authorities are changing strategy and will no longer test everyone suspected of COVID-19.
The article continues below.
By Bente D. Knudsen
The strategy to combat the coronavirus epidemic is changing these days and it will be felt by all who start feeling ill, or have symptoms that could be the virus.
The strategy of the Danish health authorities has so far been a strategy of containment – finding those infected with the virus by testing them and putting them and their close contacts into quarantine.
This was the so-called inddæmningstategi as described in the Coronavirus Strategy Document published by the authorities.
Find link here.
This strategy is now changing into the mitigation strategy, in Danish afbødningstrategi.
The article continues below.
This means that the focus of the authorities is no longer on finding all those with symptoms and testing them to ascertain if they have the COVID-19 virus.
Instead, the health authorities acknowledge that the virus has now spread from person to person in the Danish society and the focus is now on identifying those at risk and taking the necessary precautions to alleviate the effect of the virus on them.
“ The new strategy means that we are changing focus; instead of focusing on all those who have been travelling to areas of risk and who have mild symptoms, we will instead have a great focus on those who get so ill from the virus that they will need medical help.
This means that patients with light symptoms are to stay at home and will not be tested for coronavirus whereas those with severe symptoms are to call their GP. The GP will then access their state of illness ( Editor’s note: and their risk of severe effects of the illness depending on risk profile) and decide which further measures are to be taken,” says Helen Bilsted Probst, from the Danish Health Board.
The article continues below.
If a symptomatic person is high risk that person will be tested for COVID-19 so the authorities can determine if further intervention (hospitalisation) might be necessary.
This means that if you are exhibiting coronavirus-like symptoms: fever, coughing, muscle pain, you will NOT be tested for the coronavirus if you are a normal healthy person or child and your general state of health and the symptoms of your illness are mild or moderate.
This new strategy means that the authorities will refrain from using resources on people who are not in the risk group and who do not have any serious symptoms (respiratory problems for instance are severe symptoms).
The article continues below.
This is equivalent to what many expats call the “Panodil Strategy” when having a bad cold or the flu during the winter season in Denmark: the “take a panodil” and stay in bed response from their GP.
They will be finding it again if they are not a group at risk or if the symptoms are not severe (respiratory problems for instance are severe symptoms).
The normal precautionary measures of staying in bed and at home, avoiding close contact with other people, coughing into your sleeve and washing and disinfecting hands is what such a person must do in order to avoid further spread.
Creating more capacity in the medical system for coronavirus patients in the risk group – read more below.
Creating more capacity in the medical system for coronavirus patients in the risk group
In Denmark, all elective (not immediately necessary) operations and ambulatory treatments or examinations at hospitals that are not evaluated as life necessary have been suspended.
Normally there is a patient guarantee of treatment within 30 days, the so called “behandlingsgaranti”. This has been suspended until further notice.
This means that only those whose treatments at the hospital cannot be postponed will continue to be scheduled; such as cancer patients or patients with life threatening diseases or needed hospitalisations, pregnant women in labour. All others will be cancelled ( de facto postponed).
The hospitals are working on identifying those they can postpone to a later date.
The article continues below.
All Danish hospitals are revising their contingency plans and beginning to prepare more wards that can handle critically ill patients as well as installing more intensive care units.
The biggest challenge concerning intensive care units (ICUs) is not related to equipment but to having enough personnel with the qualifications needed to operate and supervise intensive care patients.
Søren Brostrøm from the Danish Health Board said at a press meeting that the authorities have started calling in personnel who recently retired and who are trained in intensive care as well as training personnel who already have some intensive care skills and who with an intensive care “crash course” will be able to care for a patient in an intensive care unit under supervision by someone fully trained in intensive care.
“These are measures which the Italian hospitals have been using in order to increase their intensive care capacity and which the Danish authorities are learning from,” he said.
Hospitals are also working on reducing or triaging follow-up ( post-op) appointments to other facilities.
The article continues below.
“More telephone check-ups will be used, sending patients to specialised doctors or their GPs, this can free up considerable capacity at the hospitals and enable the transfer of medical personnel to care units instead,” Søren Brostrøm said.
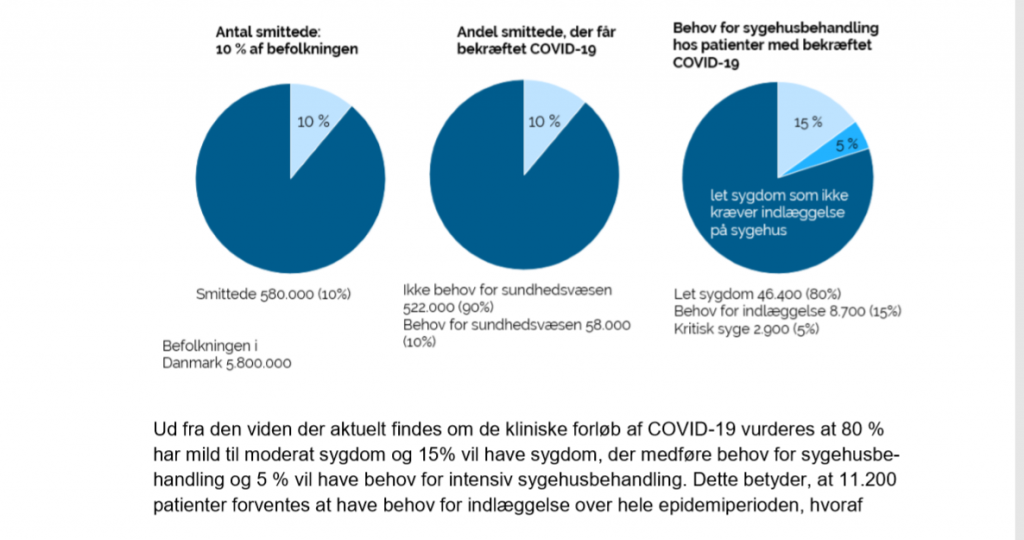
The Danish authorities are expecting that 10 percent in Denmark will be sick with COVID-19 in this first outbreak which is expected to last three months, with a peak in the middle month.
This is the calculation based on the measures taken now to both contain spread (limiting personal contacts, closing schools and universities, reducing events to less than 100 people, closing all public offices and institutions, enforced hand hygiene measures etc.) and implementing the alleviation strategy.
The article continues below.
The virus is expected to come back in October for a second outbreak, this is expected to be less significant but still serious. Those who had the virus now will be more immune to the disease.
In this first outbreak, of the 10 percent who become ill, 1 percent are expected to need some kind of medical help.
This means that approximately 60,000 Danes will need help from the medical system over a period of three months.
Based on the knowledge available, it is expected that 80 percent will only be moderately ill, 15 percent will need to be hospitalised and five percent will need intensive care treament.
This translates to a figure of 11,200 patients who will need hospitalisation over the next three months. Approximately 2,800 will need intensive care.
The article continues below.
The estimated rate of death of COVID-19 is between 0,3 to 1 percent with large variations between age groups (those above the age of 80 could be up to 15 percent mortality rate).
Between 1,500 and 5,600 patients are estimated to die from the virus in Denmark.
“It is expected that the Danish Health System will be able to implement efficient measures which will make it possible to keep the mortality at the low end of the above figure.”
The article continues below.
Above picture is from the Coronavirus Strategy Document as published by the Danish Health Board. Find the link here.
The 10 percent estimate of sick people in the first outbreak is based on several things according to the Danish Health Board: past epidemics, the general state of health of the population, the age groups ratios for instance the size of the old population in percent of the total population and what they call the worst case scenario from the cruise ship in Japan, The Diamond Princess, which had 20 percent infected in a situation where the hygiene and quarantine facilities on board were not adequate to contain spread.